Why “Ineffective” Techniques Still Help
What The Dark Side of Musculoskeletal Care Gets Right—and What It Misses
I recently received this comprehensive review, “The Dark Side of Musculoskeletal Care,” from a colleague and they wanted to know what I thought of this paper. I love that he asked for my thoughts on this and have taken a lot of time to reflect on this article and its response.
In the above linked review they examined 25 years of research on two of the most widely used complementary and alternative therapies (CAMs)—osteopathy and chiropractic care. (Don’t for a moment think that because this review was done on those two disciplines it does not apply to massage therapy, physical therapy, acupuncture or ANY OTHER version of manual therapy. It almost certainly applies equally to all manual therapies.) The authors evaluated biological plausibility, clinical effectiveness, and the mechanisms that might explain why these therapies appear to work.
The paper is well-designed and methodologically solid and I really enjoyed reading it. It offers a thoughtful critique of the biomedical explanations commonly attached to CAM approaches. It is not the first paper to reflect on the biomedical explanations, nor will it be the last. I enjoyed however, how the paper integrated the non-biomedical possible explanations, I found this wonderful to see and read.
I was engrossed in the reading until I came across its final conclusion—that these practices “cannot be recommended” for musculoskeletal care. Not because that is their conclusion, I can understand how they came to that conclusion, but rather because that conclusions seem to lean too heavily on biological plausibility and undervalues what the paper itself repeatedly acknowledges: non-specific, contextual, psychological, and emotional factors seem to produce real, measurable improvements for patients.
The paper reminds me of a scientific, statistical approach opposed to a patient/client approach. The client is seeking improvement, that is all they are after. The what, how and why of it are great to know but for less valuable than the improvement. That is what they are seeking, not the mechanism. This paper forgets the patient I think and only thinks of the evidence.
As massage therapists who practice within the biopsychosocial model daily, this raises an important question: If a treatment reduces pain, improves mood, increases function, and does so with low risk—even if the biological mechanism is unclear—should it be dismissed?
In many ways, the paper’s own findings suggest the opposite. The review shows that the biological mechanisms of osteopathy and chiropractic are weak or unsupported. (Again, feel free to replace osteopathy and chiropractic with manual therapy.)
The paper details why many traditional explanatory models—cranial suture motion, visceral manipulation, “vertebral subluxations,” etc.—lack scientific backing. For example:
Cranial “mobility” is smaller than MRI resolution, making it unlikely to be felt or therapeutically manipulated.
Viscerosomatic pathways exist, but not in the deterministic, structural way often claimed.
Vertebral subluxations are not reliably detectable or specifically treatable; spinal manipulation cannot target individual segments. (One of my favourite chiropractors even spoke about this at the past Canadian Massage Conference in Saskatoon this past September, Dr. Nikita Vizniak.)
From a purely biological viewpoint, these mechanisms fall into what the article calls the “believer’s error”—inferring causation without evidence. (If manual therapists were truly honest with themselves we would see that we are all guilty of this.) Yet patients consistently report improvements so something else is happening…but what?
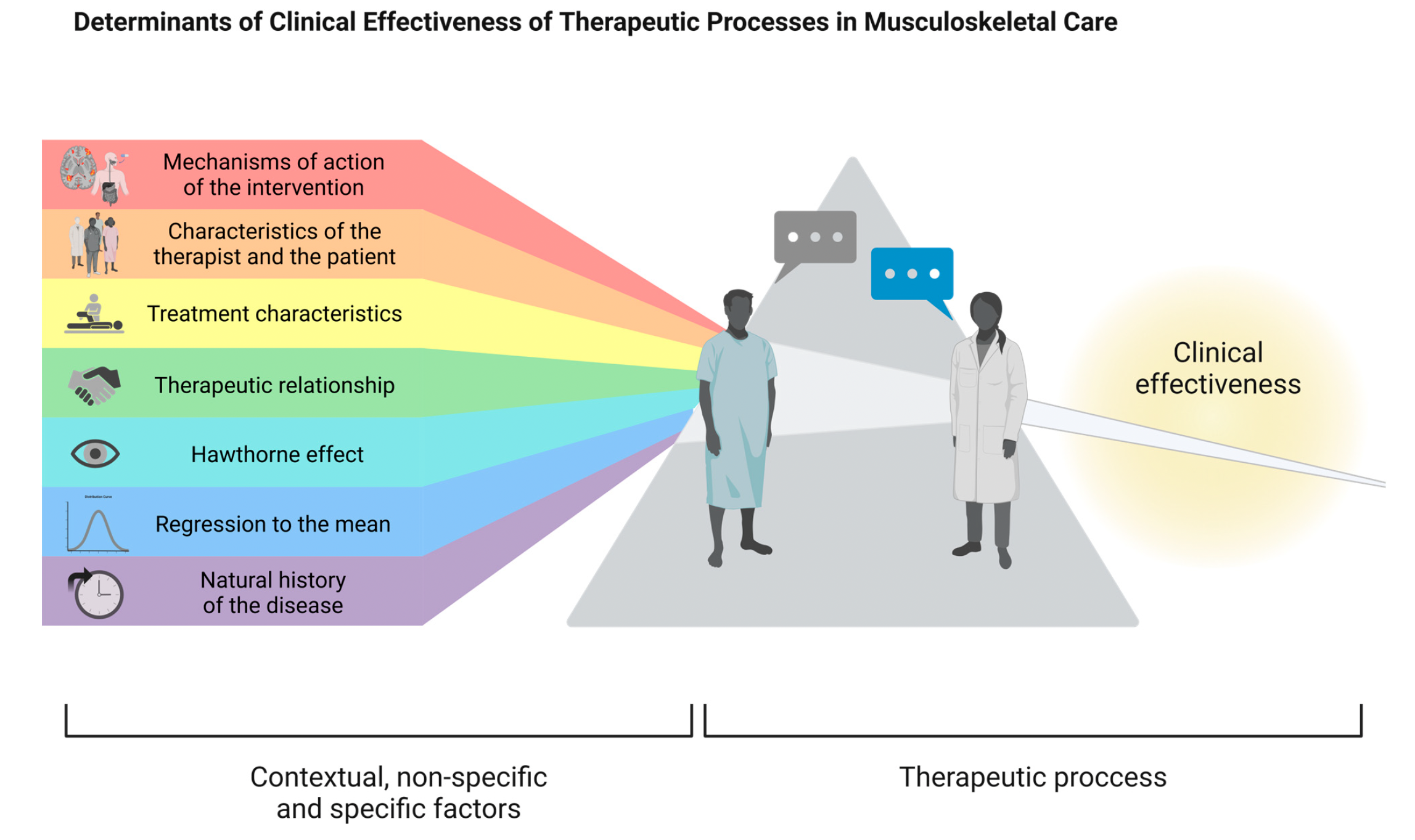
The review highlights that contextual and non-specific factors (what I call the theatre of therapy) play a powerful role in clinical outcomes:
Placebo and meaning responses
Expectations and predictions
Therapeutic alliance and communication
Attention, care, emotional support
Touch and manual interaction
Social and community belonging
Cognitive reframing and new narratives about pain
Biases that shape perception—authority, confirmation, optimism,
Barnum effect -occurs when individuals perceive vague and generic descriptions as highly accurate and personalized
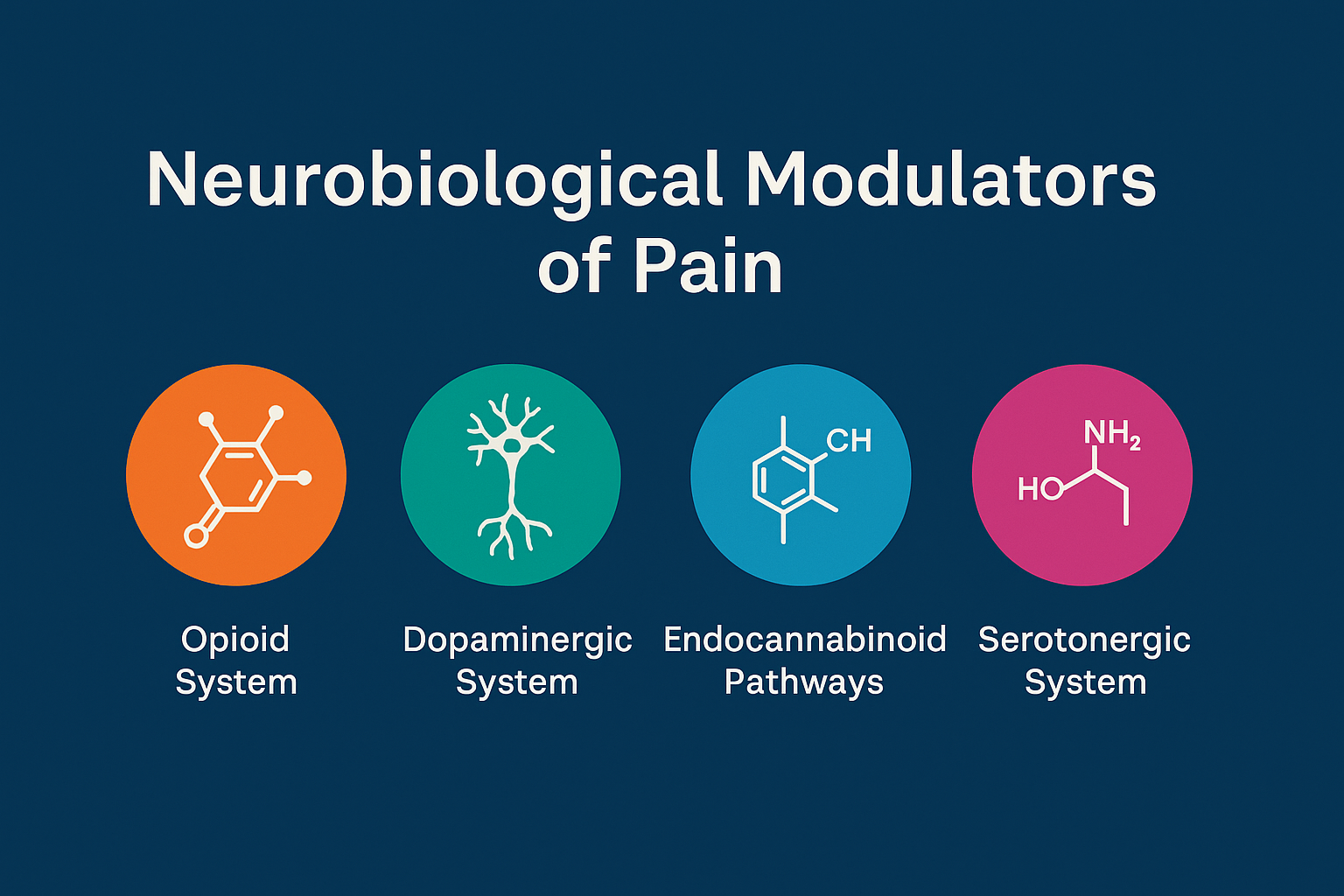
These factors are not trivial. They are neurobiological modulators of pain via:
the opioid system
the dopaminergic reward system
endocannabinoid pathways (This system is crucial for maintaining homeostasis and plays a vital role in regulating mood, pain, sleep, appetite, memory, and other functions)
serotonergic emotional-regulation systems (The neural networks in the brain that use the neurotransmitter serotonin to control mood, emotional responses, and behavior.)
cholecystokinin (CCK) interactions influencing placebo/nocebo
In reported studies, positive expectations alone produced hypoalgesia in targeted regions; negative expectations produced localized hyperalgesia. Context shaped outcomes more predictably than the intervention itself. This aligns with modern pain neuroscience—and with what manual therapists see clinically every day.
It is important and valuable to remember as well that clinical outcomes of osteopathy and chiropractic (manual therapy) are modest but meaningful!
Systematic reviews found:
No strong evidence for specific mechanisms.
Manual care often performs no better than sham when measured mechanistically.
But patients often feel better, move better, and report meaningful improvements.
And this is exactly the paradox the paper explores: how if the mechanism is weak are the outcomes still positive? The paper does not answer this by the way. It shines a light on one of the most confusing and easily most frustrating parts of manual therapy. If we don’t know the how can we still justify the outcome and more importantly in my opinion, if the outcome is there, should do we need to know the how? In short, as Matt, Justin and Anna told me in Dallas at the AMTA National Convention this past year, “Massage works!”
Here is where the I find the paper’s conclusion falls short. Despite acknowledging the contextual and psychological factors: reduced pain, improved well-being, modulated neurobiology and support of meaningful change…the authors conclude that CAM techniques “cannot be recommended” simply because the biological mechanism is unproven.
This seems asinine and counterproductive to me. A version of therapy with low risk intervention, low cost, and consistent subjective benefits should not be excluded solely on the grounds that we can’t yet explain how it works biologically—especially in a field like pain, where context seems to effect biology. (I understand that the inherit risks of manual therapy are first and most importantly, delayed appropriate care. This is something that needs to be addressed in the manual therapy field. I also understand that socioeconomic impacts make spending resources on CAM therapies potentially harmful. I do not think these risks supersede the potential benefits offered by CAM therapies.)
For massage therapists working within a modern evidence-informed model, the papers conclusion is both overly rigid and out of step with current neuroscience. If positive outcomes occur through contextual pathways, emotional regulation, touch-based communication, expectation effects, and therapeutic alliance—these are not “fake” effects. They are legitimate neurophysiological processes. To dismiss them is to misunderstand the nature of musculoskeletal pain itself but mostly, to discount the patient/client as central to all health care interventions.